Down Low on Your Down Below: POP
June is Pelvic Organ Prolapse (POP) Awareness Month - but anytime is a good time to chat about this!
I don't think I've ever heard anyone talk about POP openly or in detail before this year. I am extensively trained and aware of movements that may or may not contribute to POP, what to avoid (typically) when working with susceptible populations, and how to create better pelvic function and support. But never have I heard causal conversion about what it is and how it feels physically and emotionally to live with POP. It's always talked about as if no one in the room actually has it and how we're going to keep it that way. It seems to be a bit taboo to talk about our "Down There"!
First off, WHAT is Pelvic Organ Prolapse?
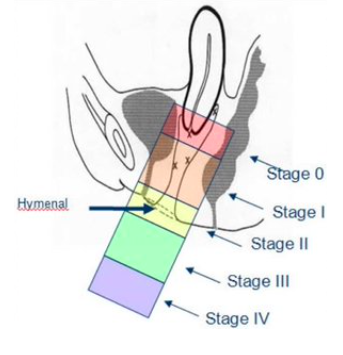
"Prolapse" refers to a descending or drooping of organs. Pelvic organ prolapse refers to the prolapse or drooping of any of the pelvic floor organs, including the Bladder, Uterus, Vagina, Small bowel, and Rectum.
In the body, the pelvic floor muscles span the base of the pelvis and support the pelvic organs. There is also support for these organs from above via connective tissue/ligaments and fascia. The pelvic organs are meant to be suspended from above and supported from below. A prolapse is likely to occur when something disrupts this balance.
(Learn more about different types of prolapse here)
Years ago, 2004 to be exact, in the immediate postpartum time after my second child was born, I realized that I couldn't tell if I had to urinate and often felt like I couldn't fully empty my bladder. I assumed it was because I had just had a baby, and her birth was wildly fast. I slowly regained sensation but continued to feel like I hadn't "finished the job."
I returned to my dance career, unable to jump. Thankfully, I wasn't in pain, but I was leaking urine; I was incontinent! Many, many postpartum bodies find themselves unable to laugh, sneeze and cough let alone jump without leaking... and I was one of them.
It was a nuisance, and I would excuse myself from class or rehearsal to use the washroom in hopes that I wouldn't all-out pee my pants. Like many of us, I thought this was just part of having had babies. I never thought to mention it to anyone, and I certainly didn't know to challenge our medical system to say this was unacceptable.
I thought it was normal. It's not. It IS common, but it's not normal.
Back then, no one talked about pelvic health during pregnancy or after giving birth. Healthcare professionals and pregnancy books alike said, "do kegels." Well, they weren't entirely wrong, but they weren't right, either.
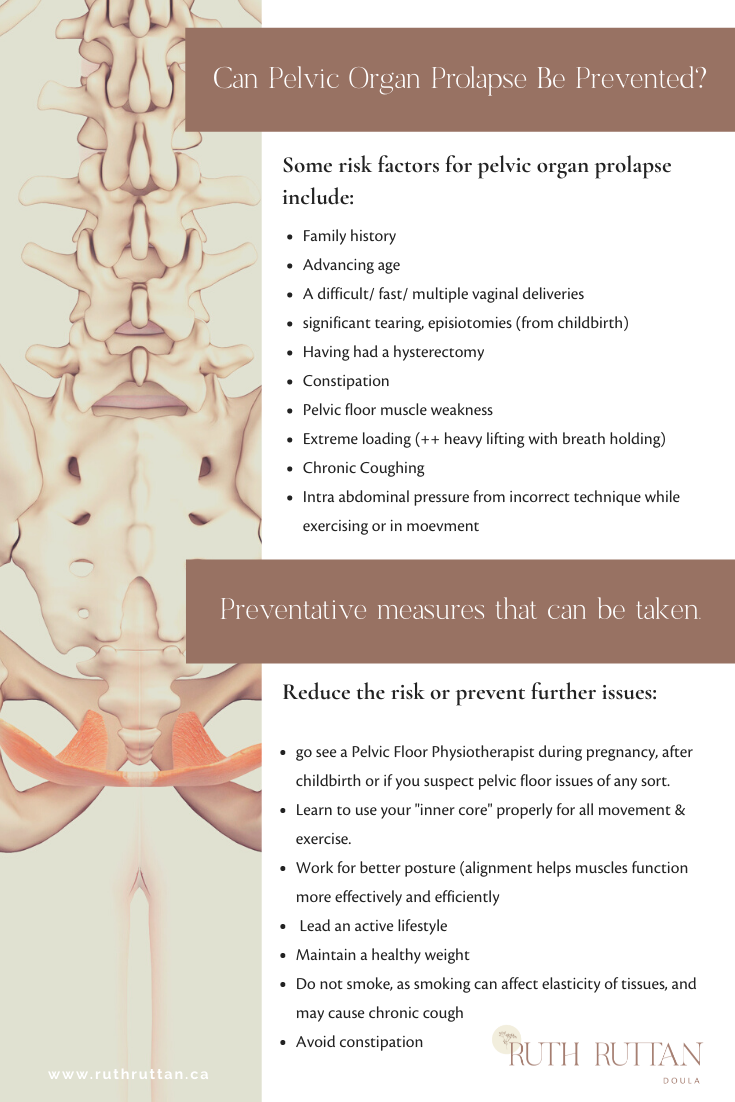
There was a considerable lack of knowledge about the contributing factors, risk factors, preventative measures and what the symptoms were. No one was telling me what to look for or that my daily physical activities, specific exercises, and postural habits may have sealed my pelvic floor fate!
This is when I began my in-depth studies on pelvic health, specifically so that I could work with pregnant and postpartum clients. I changed how I moved physically throughout my days and exercised and brought new awareness to how I taught Pilates, exercise and dance.
I thought I'd done a decent job of rehabilitating my pelvic health.
Fast forward to 2018...
Three and half years after my third baby and rehabbing a significant Diastasis Recti Abdominus, I noticed a downward pressure when I used the toilet. My bladder emptying issues came back/ seemed more frequent, and I was getting some low back pain/ ache. I booked a physical with my family doctor. About five years earlier, I had asked my doctor to check in on my pelvic health, and she poo-pooed my concerns. This time I insisted that my doctor refer me to a pelvic floor physiotherapist.
In a one-hour session, my physiotherapist congratulated me on having a excellent pelvic floor and transverus recruitment (yay! my inner core worked!) AND confirmed that I had a grade 2+ Cystocele (bladder prolapse) and grade 2 Uterocele (uterus/ cervical prolapse).
I walked home crying. It was a huge emotional blow. I can't explain why I felt so devastated and why some days, I still do. I thought I had done "all the things." After all, she said I had an excellent core! I knew now that I was "in it" for the long haul. I would always have to be aware of my symptoms and consciously try to keep them from getting worse. There was no turning back time or "fixing" this. I might be able to see measurable improvement, but more likely, the best I can hope for is to train and work toward symptom-free physical exertion. I felt like I'd failed myself.
I spend my days working on posture, breathing, and effectively recruiting and releasing my inner core, specifically focusing on PROPERLY doing a "Kegel." I integrate this with walking, sitting, and standing, and I'm working on deep squatting - all things I need to be able to do in my life and my profession. (All things I do with my clients too!) I'm more susceptible to injury and worry I'll hurt myself, and I never stop thinking about it. It's exhausting. I'm constantly thinking that my parts will fall out of my body and contemplating whether or not I should get sized for a pessary, use estrogen creams or if I'll require surgery.
In recent years, more research has gone into pelvic floor dysfunction and pelvic organ prolapse. We have a much better sense of the importance and impact our pelvic floor health has on the quality of our lives. Stay tuned for more blogs on these subjects!
Thankfully, Pelvic Floor Physiotherapists are popping up all over the place, as are Pilates Specialists (like myself) who are trained to help one reintegrate movement, build strength and better function. Even doctors and midwives are more aware of pelvic floor health and direct clients to these services.
I hope this information will decrease your chances or help you catch your issues early!
Treatment for pelvic floor dysfunction and prolapse is individualized and can be effective if it's timely and targeted. Please seek out assessment and guidance if you are pregnant and as part of your 6-week postpartum checkup (anytime after the birth of a child - the sooner, the better!) or if you have any of the symptoms listed.
If you are in the Greater Toronto Area and looking for a Pelvic Floor Physiotherapist, here’s a list of physics in your area!
If you want to know more about Pelvic Floor Health and how to exercise and function safely throughout your pregnancy and postpartum year, contact me & sign up for the newsletter here!